Results
Verify insurance eligibility and benefits
Estimate patient responsibility accurately
Prevent registration errors that cause denials
Reduce manual portal lookups
Enable quicker point of service collections
Works with major clearinghouses
Integrates with EHR/PMS systems
Automates benefit enrichment
Parsing documents and auto reporting
Supports multi-location and multi-payer workflows
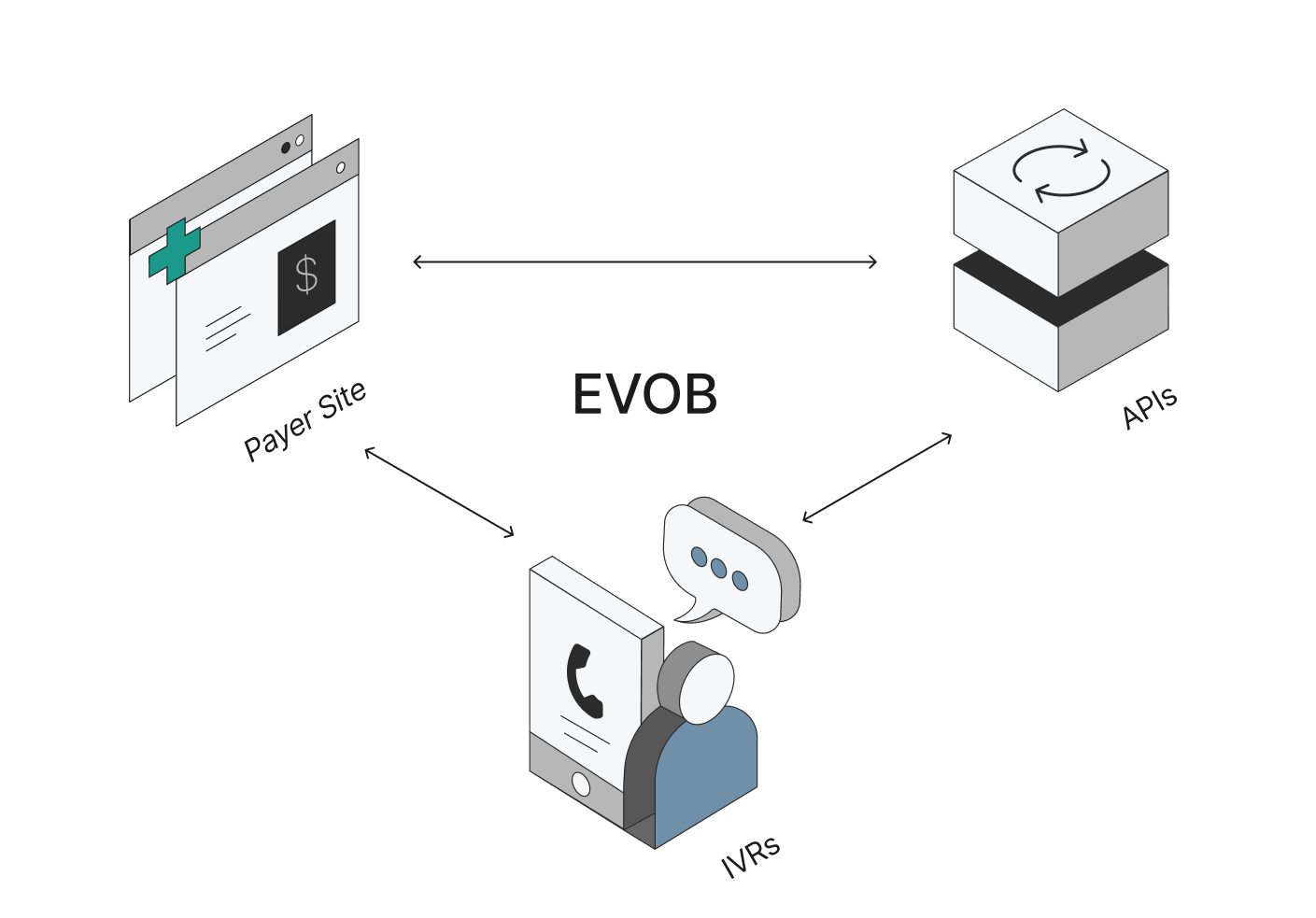
Flexbone EVOB Process
Attempts verification across insurance portals, 270/271, and voice automatically. When one method fails, Flexbone can route to the next option.
Goes beyond basic eligibility to extract detailed coverage information, enabling accurate patient responsibility estimates at intake.
Complete benefit information at intake helps you make informed decisions about patient acceptance and reduces surprise denials.
View the data in Flexbone for easy referral, with our AI agents saving all information that the insurance gave.



.png)