
Insurance Eligibility Verification in Healthcare
Insurance eligibility verification is one of the most important steps in the healthcare revenue cycle. It’s the process of confirming that a patient’s insurance coverage and benefits are valid before care is delivered. This single step determines whether a claim will be accepted, how quickly a provider is paid, and how clearly a patient understands their financial responsibility.
At its core, eligibility verification ensures three things: the patient’s insurance plan is active, the planned services are covered, and all parties, including the provider, payer, and patient, have the right information before treatment begins.
Why Eligibility Verification Matters
Eligibility verification does more than confirm whether an insurance card is current. It protects the financial health of providers and creates a transparent experience for patients.
When done correctly, it ensures that billing is accurate, claims are submitted with the right details, and payments flow without interruption. Patients benefit, too, because they know upfront what their plan covers and what costs they might owe.
For healthcare organizations, this process also supports compliance with industry regulations, reduces staff time spent reworking denials, and strengthens trust between providers and patients.
How the Process Works
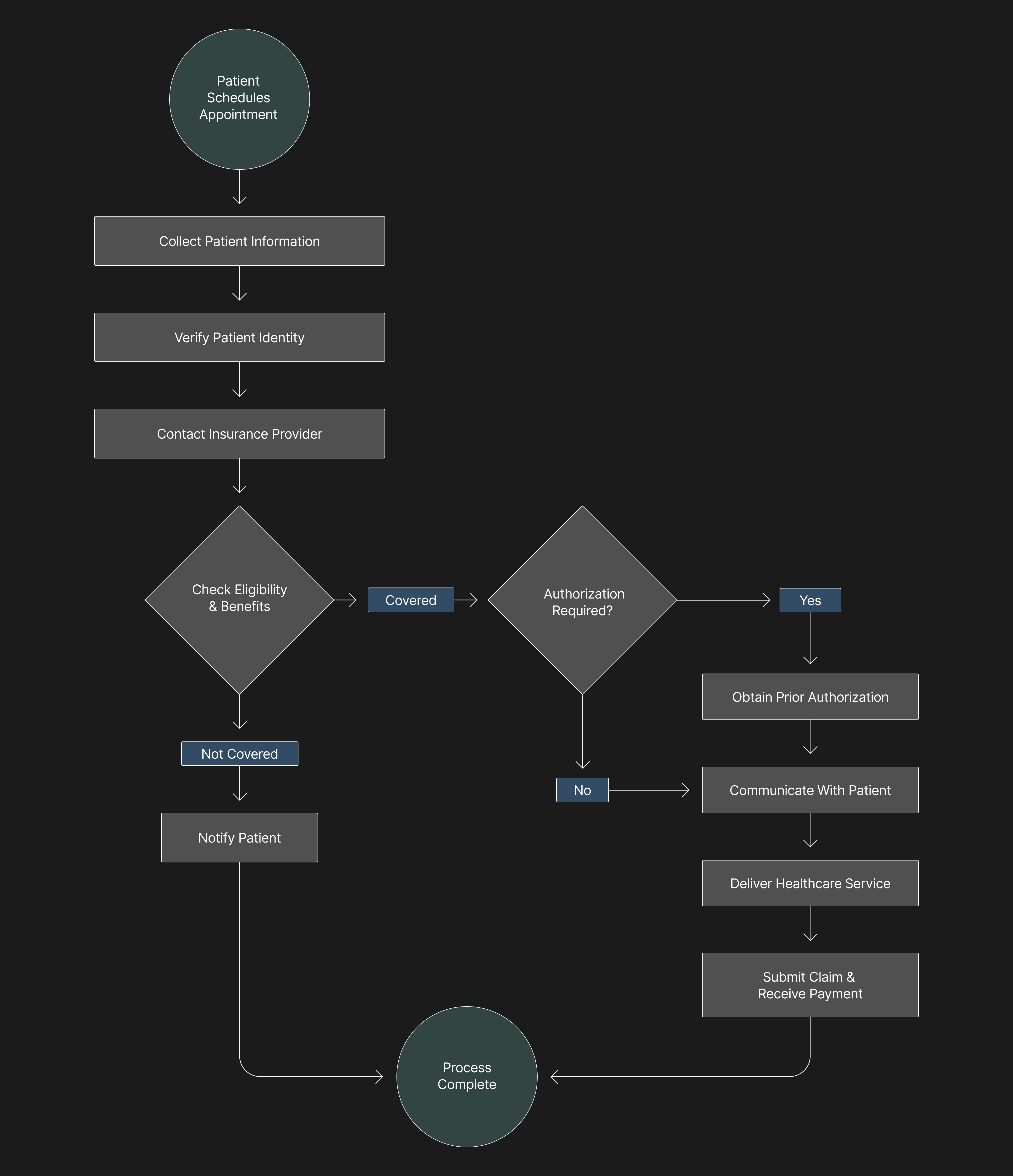
The eligibility verification process begins long before a patient steps into an exam room. It typically happens during scheduling or registration, and includes several critical steps that together form the foundation of clean billing:
- Collect patient information. Administrative teams gather demographic and insurance details such as policy number, group number, and the name of the policyholder. Every field must match exactly with the payer’s records to avoid rejection later.
- Verify patient identity. Confirm the patient’s identity using their insurance card, government ID, or past records. This prevents fraud and ensures benefits are applied correctly.
- Contact the insurance provider. Staff or automated systems reach out to the payer through phone, web portals, or clearinghouses to confirm coverage and benefits.
- Verify eligibility and benefits. Confirm whether the services are covered, identify deductibles, co-pays, and out-of-pocket limits, and check if pre-authorization is required.
- Obtain authorization when necessary. Some services or procedures require prior approval before care is provided. Missing this step can lead to automatic claim denials.
- Update patient records. Once verified, all information should be documented in the electronic health record and billing system to ensure consistency across departments.
- Communicate with the patient. Finally, the results of verification should be shared clearly. Patients need to know what is covered, what isn’t, and what they may owe.
Each step builds on the one before it. When any part is skipped or rushed, the result is often claim rework, delayed revenue, and unnecessary confusion for the patient.
Common Mistakes to Avoid
Eligibility verification sounds straightforward, but small oversights can have big consequences. Common pitfalls include verifying coverage too late, using outdated insurance details, or failing to obtain prior authorization. Even a single digit entered incorrectly in a policy number can cause a claim to be rejected.
Another frequent mistake is failing to communicate verification results to patients. When patients do not understand what their insurance covers, it can lead to frustration and unexpected bills later. Regular communication ensures that financial discussions happen before care, not after.
Key Benefits of Accurate Eligibility Verification
When done correctly, eligibility verification creates a smoother experience for everyone involved.
For healthcare providers, it means:
- Fewer denied or delayed claims, since coverage details are correct the first time.
- Improved cash flow, with faster payment cycles and less administrative follow-up.
- Stronger compliance with privacy and billing regulations, including HIPAA.
For patients, it provides:
- Clear understanding of coverage, co-pays, and out-of-pocket costs.
- Fewer surprise bills or payment disputes.
- Greater confidence in the billing process and the healthcare provider.
The result is a system where both accuracy and trust improve over time.
The Role of Technology and AI
Modern technology has made it possible to verify insurance eligibility instantly across hundreds of payers. Instead of manually checking individual portals, automated systems connect directly to payer databases and return structured, real-time responses. This reduces administrative workload and ensures consistency.
Artificial intelligence takes this one step further. AI systems can recognize subtle changes in payer portals, flag inconsistencies in returned data, and adapt when formats or requirements shift. Rather than failing silently, they can alert staff when human review is needed.
At Flexbone, AI plays a central role in making eligibility verification more dependable. Our systems are designed to:
- Validate each step of the process automatically, maintaining full transparency.
- Scale across different payers, networks, and systems without losing accuracy.
- Continuously learn from new data to identify patterns that cause denials.
This kind of automation doesn’t just make the process faster: it makes it smarter, more accountable, and easier to trust.
The Bottom Line
Insurance eligibility verification may seem like an administrative detail, but it is one of the most important safeguards in healthcare operations. It keeps claims accurate, payments consistent, and patients informed.
By combining standardized processes with advanced automation and AI, healthcare organizations can build systems that verify coverage accurately, adapt to constant change, and maintain transparency at every step.
Eligibility verification isn’t just a step in billing; it’s the start of a reliable, trusted healthcare experience.
Connect With Us
We are here to help you with any questions. Drop a line and our team will get back to you as soon as possible
Get In Touch



.png)